03.12 GI/GS – Jaundice
Physiology / Pathophysiology
= Yellowing of the skin secondary to raised bilirubin
Bilirubin levels need to be >50 µmol/L to produce clinically significant jaundice (ref)
Doesn’t seem to matter which fraction of bilirubin is raised
Bilirubin
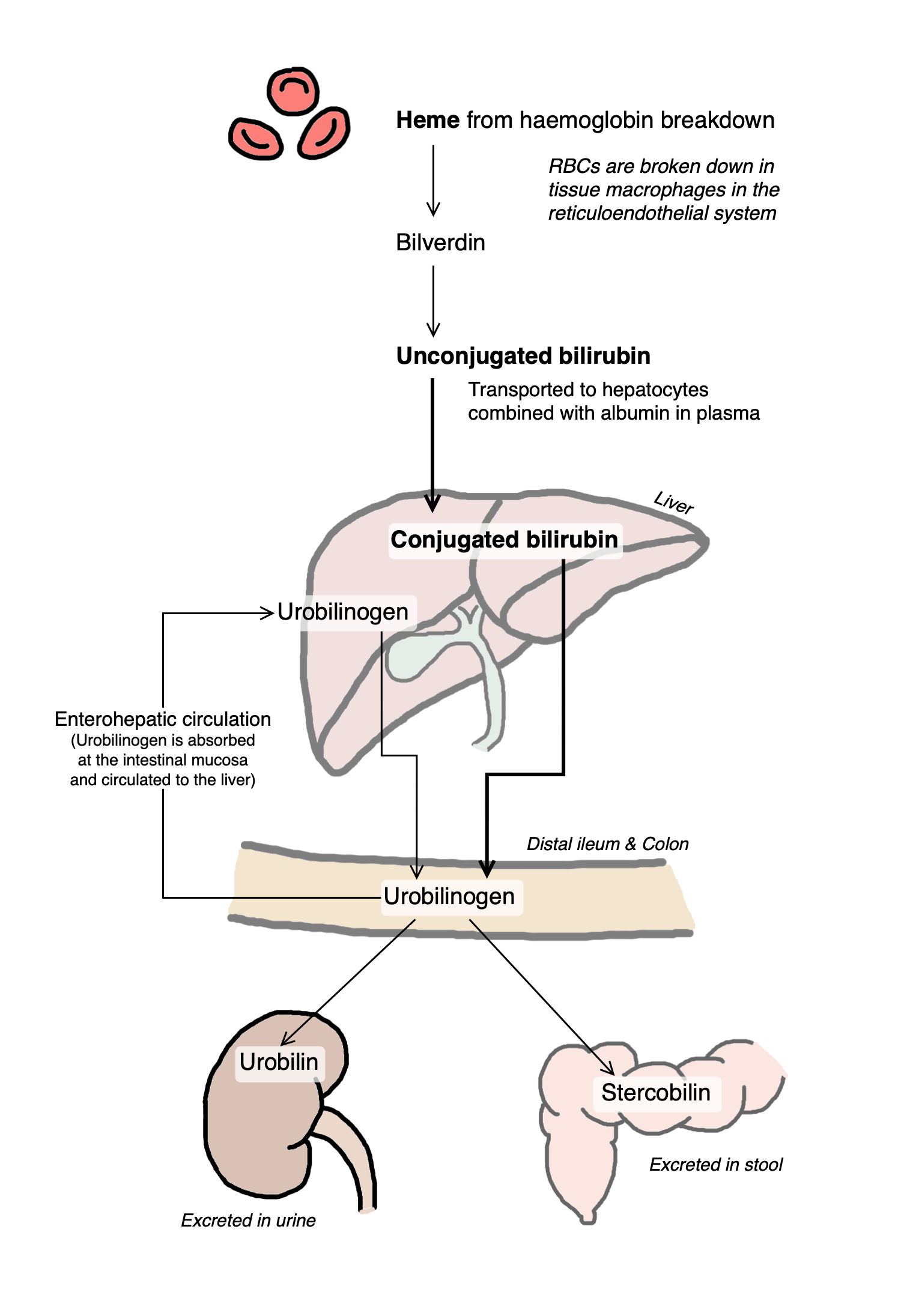
Unconjugated bilirubin (UCB) is produced as a result of heme metabolism
UCB is insoluble, and is transported to the liver attached to albumin
UCB is converted to soluble conjugated bilirubin (CB) in the liver
CB is released into bile, which is then excreted from the body via the gut or kidneys (see diagram)
Raised levels of UCB or CB will result in hyperbilirubinaemia
Lab results usually note total bilirubin which includes both fractions
Direct bilirubin is an estimate of conjugated bilirubin – this has to be specifically requested on forms
Indirect bilirubin refers to unconjugated bilirubin
Causes of jaundice
Causes of jaundice can be broken down into pre-hepatic, intra-hepatic, and extra-hepatic.
Pre-hepatic jaundice
Pre-hepatic jaundice is caused by disease processes occurring before the liver; pre-hepatic jaundice is therefore related to a rise in unconjugated bilirubin.
Raised unconjugated bilirubin can be due to increased red blood cell breakdown, i.e., haemolytic anaemias.
Examples of these include hereditary spherocytosis, sickle cell anaemia, G6PD.
Raised unconjugated bilirubin can be due to reduced rate of conjugation,
An example of this is Gilbert syndrome, where there is a genetic defect resulting in lower levels of a specific enzyme required for conjugation of bilirubin (Wikipedia). Gilbert syndrome is benign, and jaundice only happens intermittently when the body is under increased levels of stress.
A more severe example is Crigler-Najjar syndrome, an autosomal recessive disorder resulting in defects in a specific enzyme required for conjugation of bilirubin. Type I requires liver transplant as a cure, while Type II can be managed with phenobarbitals
Intra-hepatic jaundice
Intra-hepatic jaundice is caused by [1] damage to the hepatocytes where conjugation of bilirubin occurs (≈ hepatitis), or [2] obstruction within the liver (= cholestasis).
Examples of damage to hepatocyte / hepatitis include viral hepatitis, alcoholic hepatitis, autoimmune hepatitis – all of which can result in cirrhosis.
Disease processes causing cholestasis include primary biliary cholangitis and Dubin-Johnson syndrome.
Hepatotoxic drugs can cause drug-induced liver injury (DILI) – either damage to hepatocytes, cholestasis, or both [see more comprehensive list in article here].
Hepatocellular damage: paracetamol(!), valproate, isoniazid, rifampicin, pyrazinamide, amiodarone, nitrofurantoin, etc
Cholestasis: COCP, amoxicillin & co-amoxiclav, flucloxacillin, co-trimoxazole, clarithromycin, erythromycin, etc
Extra-hepatic jaundice
Extra-hepatic jaundice is caused by obstruction preventing bile from being transported from the liver to the intestines.
Examples include gallstones in the common bile duct, cholangitis, primary sclerosis cholangitis, cholangiocarcinoma, and disorders causing extrinsic compression of the common bile duct (i.e., Mirrizi syndrome) such as pancreatic cancer or pancreatitis.
Clerking for jaundice
PC: Jaundice
HPC:
When did they first notice jaundice?
First episode? Comes and goes?
Ask about associated smx:
Abdominal pain
Abdominal swelling
Nausea, vomiting
CIBH – constipation / diarrhoea
Colour of stools
Any one else in the family sick?
PMH:
DHx:
Recent change in medications?
** Check for interactions
Allergies:
FHx:
SHx:
Alcohol
Smoking
Illicit drug use – IVDU?
Recent travel? (possibility of hepatitis)
Living situation
Obs: NEWS
Investigations
Bloods: LFTs
ECG:
CXR:
Other imaging
O/E
Check for stigmata of liver disease (see GeekyMedics)
Plan
Immediate investigations (which can be done before senior review)
- Add on (or doing) full set of LFTs (incl direct bilirubin, ALT & GGT)
- Viral hepatitis screen (± BBV, EBV & CMV serology if at risk)
Further investigations depending on senior review / further development of jaundice and disease process
- Non-invasive liver screen (NILS) may be required for chronic liver disease (see below)
- Imaging depending on cause: USS liver, MRCP/ERCP, CTAP / CT abdo
- Ascitic tap if applicable (send for biochem, cytology and MCS)
- Biopsy
Management will depend on cause of jaundice
Non-invasive liver screen (NILS) – basically bloods that include the following (send 1x gold top + 1x blue top + 1x red top):
LFT (including AST), clotting screen (INR), ferritin
IgA-TTG, immunoglobulins (electrophoresis)
Autoimmune profile, including ANA, ANCA, RF [to be updated]
Cholesterol
Hepatitis bloods – Hep A antibodies, Hep B (Hep B surface antigen & core antibody), Hep C antibodies
References
Daniel S. Pratt, Chapter 73 - Liver Chemistry and Function Tests, Editor(s): Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt, Sleisenger and Fordtran's Gastrointestinal and Liver Disease (Ninth Edition), W.B. Saunders, 2010, Pages 1227-1237.e2, ISBN 9781416061892,(https://www.sciencedirect.com/science/article/pii/B9781416061892000731)
Kalyan Ram Bhamidimarri, Eugene Schiff, Drug-Induced Cholestasis, Clinics in Liver Disease, Volume 17, Issue 4, 2013, Pages 519-531, ISSN 1089-3261, ISBN 9780323261067, https://doi.org/10.1016/j.cld.2013.07.015.
